Pendred Syndrome
Definition Of Pendred Syndrome
Pendred Syndrome is a genetic condition which is associated to having a hearing loss (presbycusis) and a thyroid condition (goiter) which is common to children. This condition not only affects the auditory and gland functions but it also affects the balance due to the affected vestibulocochlear area. The hearing loss is characterized to be severe to profound bilateral sensorineural hearing impairment. It is usually congenital but non-progressive. [1][2][3]
Origin Of Pendred Syndrome
The congenital condition was named after the famous physician, Vaughan Pendred. He is an English doctor that described the condition from an Irish family in 1896. He then found out and diagnosed that cases of congenital deafness was in total of seven point five percent (7.5%). [6]
Causes Of Pendred Syndrome
The syndrome is noted to be a genetic disorder leading to the cause of coming from a genetic dysfunction or altered development during fetal development manifesting in childhood years.
What Gene Is Involved In Pendred Syndrome?
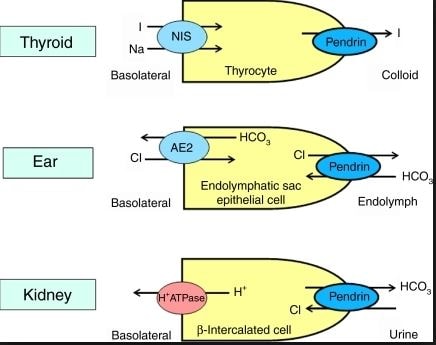
The gene that was affected from changes and altered mutations is on the chromosome 7 which is now called the SLC26A4 (formerly known as the PDS gene). This gene comprises a recessive trait to a child.
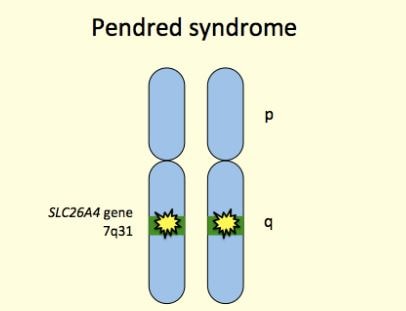
The characteristic of this gene to take effect of acquiring this syndrome, needs to have two (2) mutated SLC26A4 genes coming from each parent. Since it a autosomal recessive trait, the parents don’t manifest the disorder since they are only carriers of the genes. The effect or the signs will manifest in their children if both parents have the same gene dysfunction which becomes dominant to child. [4]
Signs And Symptoms Of Pendred Syndrome
Since the syndrome have a dominant sign the pathognomonic sign of this disorder revolves in three (3) major symptom: [4][6]
Hearing Dysfunction (Hearing Loss)
Early hearing loss or presbycusis is one of the most common characteristics of having Pendred Syndrome; but this symptom alone does not mean a child has the condition since there are other disorders and diseases that manifest the same signs.
Vestibular Dysfunction
Suspected in infants with normal motor development who episodically experience difficulty walking because of the affected balance nerve and functions.
Thyroid Dysfunction (Goiter)
Goiter is a common feature of Pendred syndrome, but many individuals who develop a goiter do not have Pendred syndrome noted. It also may be caused of other factors such as levels of iodine in the body.
Complications Of Pendred Syndrome
The patient suffers from these signs and symptoms can lead them to the following risks:
- Loss of balance
- Hearing loss
- Enlargement of the thyroid gland
- Increase risks to endangerment, accidents and injuries
Diagnosis
The patient should see to it to pay a visit to the following physicians to monitor their condition and be able to assess the severity of their disorder. [4]
- Otolaryngologist – a doctor who specializes in diseases of the ear, nose, throat, head, and neck
- Clinical geneticist – the one who specializes in considering and assessing hearing loss, inner ear structures, and sometimes the thyroid in diagnosing Pendred syndrome.
- Endocrinologist – doctors who specializes in the glandular functions of the thyroid and parathyroid glands.
They are the one who seeks objective assessments and subjective assessment to make sure that the patient is really suffering and manifesting this syndrome. [2][3]
- Objective Assessment – looking at the anatomical and physiological functions of the ears and throats of the patient.
- Subjective Assessment – asking certain and specific questions addressing the condition and signs of Pendred Syndrome.
Particular asked questions are the following:
- “When did the hearing loss start?”
- “Has it worsened over time?”
- “Did it happen suddenly or in stages?”
Laboratory Exams
Molecular Genetics Tests
- Deletion/duplication analysis
- Mutation scanning of select exons
- Sequence analysis of the entire coding region
- Targeted variant analysis
- Sequence analysis of select exons
Hearing Dysfuntion
- Magnetic Resonance Imaging (MRI)
- Computed Tomography (CT) scan
- This tests run down and look into the three (3) major signs of Pendred Syndrome. The most prominent results that is detected through these test is that of the cochlear area. [2][4]
The Cochlea
The cochlea is the spiral-shaped part of the inner ear that converts sound into electrical signals that are sent to the brain. A healthy and normal cochlea has two-and-a-half turns, but the cochlea of a person with Pendred Syndrome may have only one-and-a-half turns noted upon conduct of series of tests. However, not everyone with Pendred syndrome has an abnormal cochlea because it can also be caused by other factors.
The Inner Ear
A normal inner ear and enlarged vestibular aqueduct, showing and composed of the cochlea, endolymphatic sac, endolymphatic duct, vestibular aqueduct, enlarged vestibular aqueduct, and enlarged endolymphatic sac.
A second characteristic of Pendred Syndrome is that there is an enlarged vestibular aqueduct noted. The vestibular aqueduct is a bony canal that runs from the vestibule (a part of the inner ear between the cochlea and the semicircular canals) to the inside of the skull. Inside the vestibular aqueduct is a fluid-filled tube called the endolymphatic duct, which ends at the balloon-shaped endolymphatic sac. The endolymphatic duct and sac usually are also enlarged.
That is why many physicians and otolaryngologist do not recommend testing thyroid hormone levels in children with Pendred Syndrome, because the levels are usually normal. And the anatomical structure of the ear is shorter and lesser among children.
Thyroid Dysfunction
Perchlorate Washout Test – One f the best examination that determines whether the thyroid is functioning properly in children who suffers from Pendred Syndrome.
Prognosis And Prevalence
The prevalence of Pendred syndrome is still unknown. However, many researchers estimate that it accounts for seven (7) to eight (8) percent of all hearing loss that is present from birth (congenital hearing loss).
What Is The Life Expectancy Of Pendred Syndrome?
Patients with Pendred Syndrome does not affect the life expectancy of affected individuals. Since only organs are affected and can be palliat and rehabilitated by undergoing series of managements and treatments. Hearing aids, sign language or cochlear implants can improve the quality of life of patients by improving communication capacities which makes the patient still enjoy doing activities of daily living. [6]
Managements And Treatments Of Pendred Syndrome
The patient will not only need to go on management and treatments but the parents will also have to be part of the treatment to be able to make the child or the individual cope easily from their conditions: [4][5]
Early Surveillance and Detection Managements
- Semiannual or annual examination by a physician familiar with hereditary hearing impairment or annual visits to Otolaryngologist
- Semiannual or annual examination by an endocrinologist familiar with Pendred Syndrome
- Repeat audiometry initially every three to six months if hearing loss is progressive
- Ultrasonography with periodic reassessment at least every 2-3 years
Evaluations Following Initial Diagnosis
- Assessment of auditory acuity (ABR emission testing, pure tone audiometry)
- Thin-cut CT of the temporal bones to identify structural abnormalities
- Vestibular function studies
- Thyroid ultrasonography and thyroid function tests (T3, T4, and TSH)
- Medical genetics consultation
Treatments and Managements
- Hearing rehabilitation (hearing aids as early as possible)
- Consideration of cochlear implantation in individuals with severe to profound deafness
- Educational programs designed for individuals with hearing impairment
- Treatment of abnormal thyroid function (if present) using thyroid hormone replacement therapy
- Activities of Daily Living (ADLs)
Patient with Pendred Syndrome are not encouraged to engage to weight lifting activities and sports with increase contact and exerting too much effort.
References:
- https://ghr.nlm.nih.gov/condition/pendred-syndrome
- http://www.medicinenet.com/pendred_syndrome/article.htm
- https://www.nidcd.nih.gov/health/pendred-syndrome
- http://www.ncbi.nlm.nih.gov/books/NBK1467/
- http://flipper.diff.org/app/items/6287
- https://results.gentlelabs.com/pendred-syndrome
