Prepatellar Bursitis
What is Prepatellar Bursitis?
Prepatellar bursitis is a medical condition in which the bursa that covers the patella is inflamed. The bursa is small fluid filled sac that reduces friction as joints roll over one another.
The Prepatellar bursitis or “housemaid’s knee” (so called because housemaids spend a lot of time on their knees scrubbing floors) is common condition that arises from repeated pressure on the prepatellar bursa. With continued prepatellar bursitis, treatment may be needed to resolve the underlying inflammation.
Anatomy
To understand prepatellar bursitis management, we need an anatomic understanding of the knee and the surrounding structures.![]()
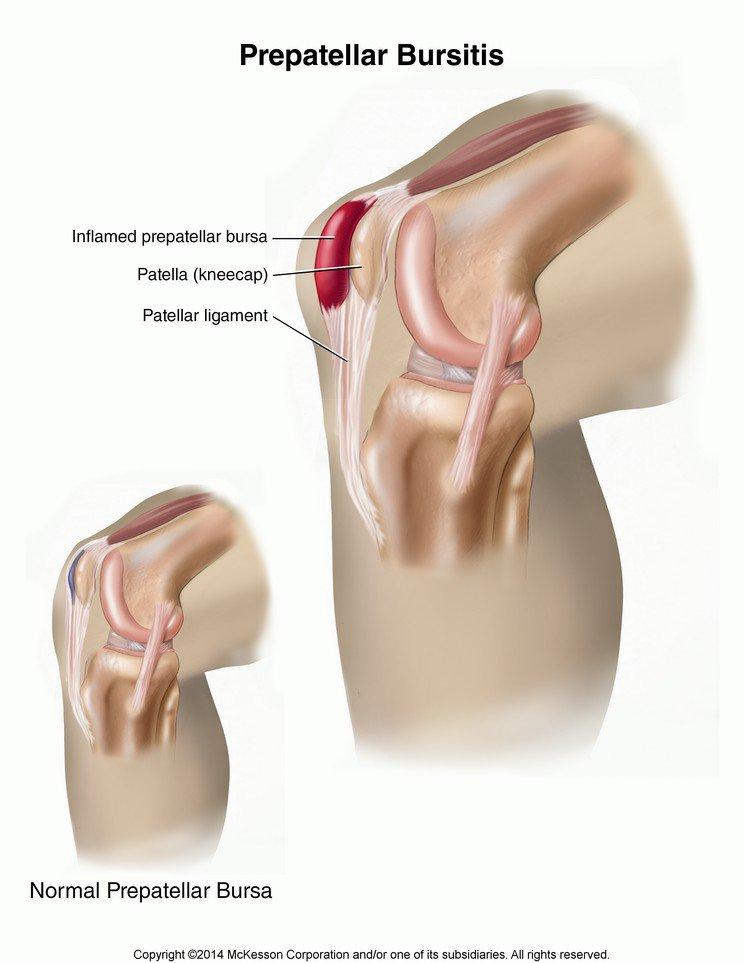
Image 1: The Prepatellar Bursitis
The Prepatellar Bursa is located just in front of the patellar bone/kneecap and separates the patellar tendon and skin. It functions to reduce friction and strain on the knee joint and acts as a cushion against high tension stretching activities of daily living such as walking, running and jumping.

Image 2: An example of prepatellar bursitis at the surface
A variety of conditions can lead to prepatellar bursitis. Prepatellar bursitis management is focused on resolving the underlying cause of the inflammation.
Direct trauma to the knee may cause prepatellar bursitis, as can recurrent minor knee injuries. Infection of the bursa can cause an inflammatory condition that is restricted to the bursa itself. Rheumatoid arthritis, gouty arthritis and various metabolic diseases can also cause inflammation of the bursa.

Image 3: A housemaid at risk for prepatellar bursitis
The people who are most at risk for this disease are people who spend a lot of time on their knees such as tile layers, carpet removers, miners and gardeners. Repeated movements that irritate the bursa are elicited in the patient’s history.
Signs & Symptoms
The signs and symptoms of prepatellar bursitis are the following
- Knee pain
- Knee swelling (pictured above)
- Redness of the knee
- Ambulation difficulties
- Inability to kneel without causing pain
- Relief of pain upon rest
- Occupational history of repeated knee movements
- Direct trauma to the knee that results into signs and symptoms 10 days after
Diagnosis
The patient’s diagnosis is confirmed with the use of an excellent history and physical examination of the affected knee. Some imaging studies can be done to visualize the extent of the damage of the knee and proper interventions can be initiated.
X-ray of the affected bursa shows very little information unless the damage has been extensive enough to include the bone. For better visualization, the imaging modality of choice is Magnetic Resonance Imaging. This imaging modality is able to show any soft tissue damage that may have occurred in the bursa to supplant the diagnosis. Aspiration of bursa fluid may be used to see if there is an underlying infection.
Once confirmed, the treatment may begin first with conservative, non-pharmacologic therapy. The RICE method which is composed of Rest, Ice Compress and Elevation of the affected extremity is effective for relieving pain. Initially, if the damage is not too great and enough time is given for the bursa to recover, the underlying inflammation subsides and the patient returns to a premorbid function.
If the damage is great and the pain and disability persists despite these conservative treatments, pharmacologic approach for management of prepatellar bursitis management is needed. Nonsteroidal, anti-inflammatory medications can be used to halt the underlying inflammation as well as reduce pain.
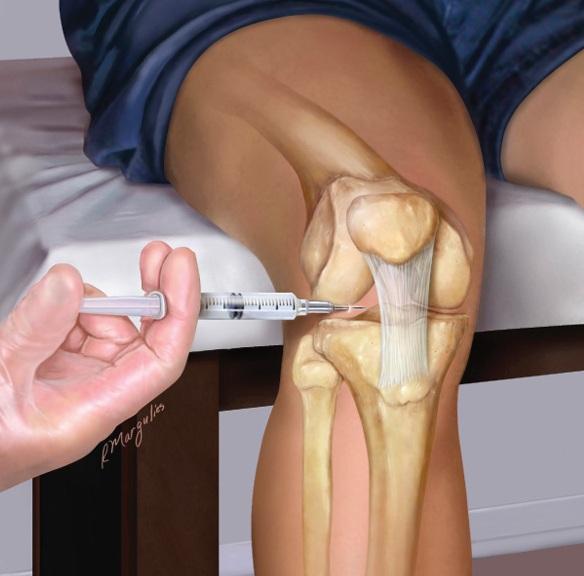
Image 4: Intrabursal corticosteroid injections for prepatellar bursitis managment
If the damage to the bursa is extensive due to repetitive insults, intrabursal corticosteroid injections can be given in place of the NSAIDs. Physiotherapy can be initiated to increase the patient’s thresholds to pain and improve performance of the affected knee.
After the prepatellar bursa is given enough rest, the patient can adapt a diet high in protein and vitamin C to increase the healing rate.
In cases of inflammatory conditions related to infection, the physician may prescribe antibiotics. If the full course of the antibiotic is followed, the patient can expect recovery in the first 3 days and follow up insured to make sure that the underlying bacterial infection is resolved.
Prepatellar bursitis management is cases of gouty or rheumatoid arthritis; dietary changes can be changed to reduce metabolites of purine that lead to formation of uric acid responsible for prepatellar bursitis. The rheumatoid arthritis can be kept in checked by a battery of immunosuppressant until the underlying infection can be resolved.
If the condition still continues even with conservative medical therapy, reassessment is needed and surgical removal of the bursa may be indicated. The surgeon opens up the knee to remove the inflamed bursa and normal function can resume once enough rest and treatment is given. The patient may need constant follow up.
Prognosis
Prepatellar bursitis has a good prognosis as long as the patients adhere to a therapeutic regimen of rest and relaxation of the affected bursa. Repetitive pressure on the prepatellar bursa causes more inflammation and may take a long time before it fully heals.
Given enough time and treatment, the bursa returns to its normal, non-inflamed state and activity can be resumed as usual. The patient is expected to have a good quality of life with the resolution of the inflamed bursa.
Conclusion
Prepatellar bursitis is common among those workers who spend a lot of time on their knees. The prepatellar bursa is responsible for reducing friction in between the tendon and the knee cap. This makes it subjected to a lot of stress in day to day activities that involve a lot of kneeling.
If not enough time is given to rest and relax these areas, the inflammation continues unabated. If conservative medical therapy does not resolve the inflammation the patient may need to have surgery.
Overall, this condition is easily relieved in a majority of patients. Most complaints are just enough for the patient to seek medical attention when the damage is substantial but not severe enough to warrant surgery.
References:
- Snell Anatomy 9th edition
- Campbell’s Operative Orthopedics 13th edition
- Current Medical Diagnosis and Treatment 5th edition
- Netter’s Orthopedic Clinical Examination 2nd edition
