Central Cord Syndrome
What is Central cord syndrome?
Central cord syndrome (CCS) is a type of incomplete cervical spinal cord injury. It was first reported in 1954 by Richard Schneider and his colleagues.
It is generally associated with favourable prognosis for functional recovery and some degree of neurological. However, factors such as age, pre-existing conditions, and extent of injury will affect the recovery process. (8)
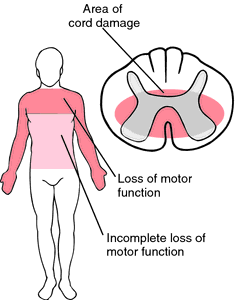
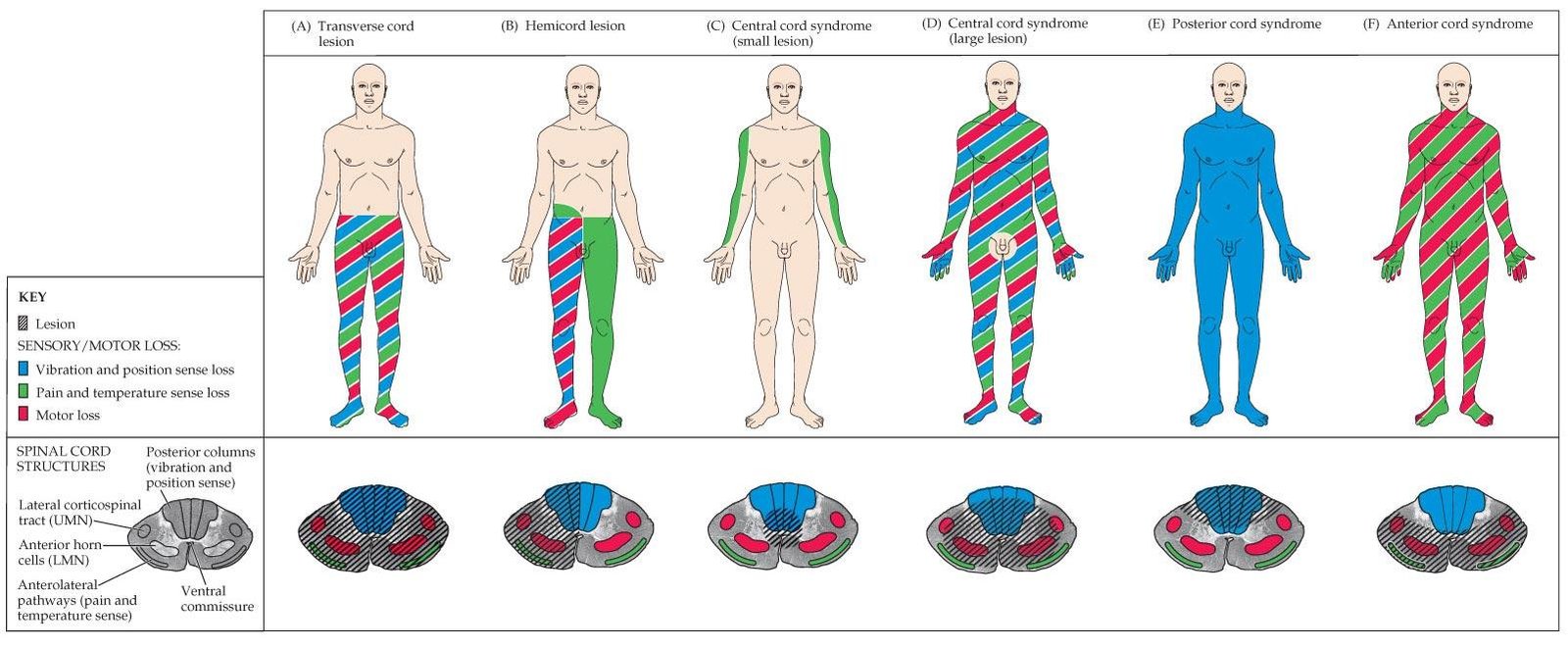
Fibres carrying the sensory and motor impulses for lower limbs are located in the most peripheral part of the cord. Sacral tracts are usually spared from injury and are located peripherally. The disproportionate motor involvement observed in this type of syndrome is due to location of nerve tracts and fibres are consistent with the lamination pattern of the tracts in the spinal cord.
Anatomy
- Sacral tracts are positioned on the periphery of the cord & are usually spared from injury
- Fibres responsible for the upper extremity and voluntary bowel and bladder function are more centrally located
- Fibres controlling the lower extremity motor and sensory functions are located in the most peripheral part of the cord
Symptoms & Signs
Central cord syndrome caused by injury can develop symptoms suddenly. Some typical symptoms and signs related to alien hand syndrome are as follows:
- Limbs weakness
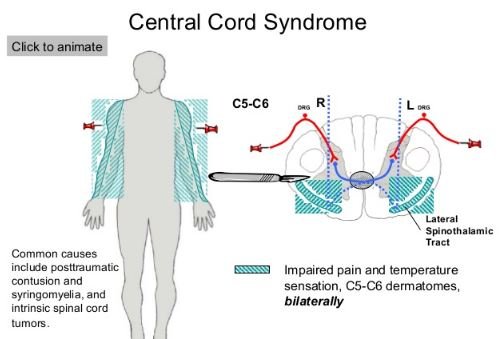
- Loss of temperature and pain sensation
- Loss of feeling
- Loss of sensation of light position and touch
- Dysfunction of bladder and often urinary retention
- Motor impairment of the upper extremities than lower
- Varying degrees of sensory loss. Spasticity, shoulder pain, hand oedema and dysaesthetic pain are noted complications
- Resulting in a flaccid paralysis due to damage to the anterior horn cells of the muscles supplied
- Gradual wasting of the muscles give rise to the central cord lesion
- Muscle weakness in legs and difficulty walking
- Numbness and tingling
- Inability to lift arms and hands
- Difficulty to button a shirt
If central cord syndrome is due to trauma, symptoms usually come quickly. However, sometimes symptoms may come more slowly.
Epidemiology
Central cord syndrome most often occurs in older persons with cervical spondylosis. It may also occur in younger persons with trauma to the cervical spine
Mechanism
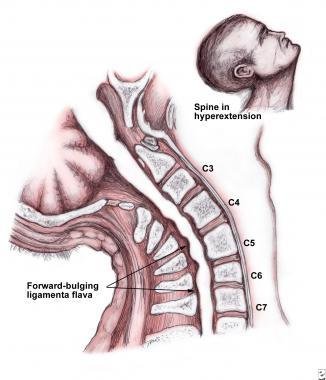
The most common mechanism for central cord syndrome is hypertension cervical spine injury. It can also be seen with other mechanisms like flexion. This type of syndrome may occasionally more chronically associated with syrinx or/and intramedullary cord syndrome. (7)
- Pinching of spinal cord between ligamentum flayum and intervertebral disc and posterior vertebral body bone spurs is caused by hyper extension injury.
- The upper motor neuron spastic paralysis of trunk and lower extremity is produced by the damage of the central portion of corticoid spinal and spin thalamic long tracts in white matter.
- Pincer effect of osteophytes anteriorly and infolded limentum flayum is produced by the impact damage to grey matter.
- The injury pattern accounts within the spinal cord tracts due to more peripheral positioning of lower extremity axons.
- The compression of adjacent white matter tracts lead to haemorrhage and central cord syndrome.
- Posterior produces severe flaccid lower motor neuron paralysis of fingers, hands and arms.
Risk Factors
The risk factors that include the chance of central cord syndrome are
- Participation in sports like wrestling and diving
- Autoimmune disorder like multiple sclerosis and neuromyelitis optic
- Narrow spinal canal, tethered cord and spinal cord disease
- Male over age of 50
The central cord by anterior and posterior compression
. 
Causes
Central cord syndrome most often occurs due to hyperextension injury in a patient with long standing cervical spondylosis. Typically this type of syndrome is also seen in younger patients as a result of a high-force trauma or a bony instability in the cervical spine.
It is usually the result of trauma to the spinal cord. The cord is pinched by an anterior compression or the ligamentum flavum by the osteophytes.Spinal cord damage was believed to originate from contusion or concussion of the cord with stasis of axoplasmic flow.
This leads to edematous injury instead of destructive hematomyelia. More recently, autopsy studies have demonstrated that central cord syndrome may be caused by bleeding into the central part of the cord, portending less favorable prognosis.
Studies also have shown from post-mortem evaluation that central cord syndrome probably is associated with selective axonal disruption in the lateral columns at the level of the injury to the spinal cord with relative preservation of the grey matter. (4)
- Trauma is the most common cause for central cord syndrome
- Significant risk factor in older patients is premorbid cervical spondylosis
- Trauma associated with cervical fracture or subluxations is observed in younger patients
- Population with a narrow spinal canal results in tetraplegia
- Loss of blood supply to the damaged area
- Spinal cord bleeding
- Swelling
- A narrow spine born due to pre-existing condition
- Spinal cord tumors
- Tructural problems
- Degenerative conditions in older patients
- Spinal cord cysts development termed as Syringomyelia
Central cord syndrome is usually caused to the central part of the spinal cord. Yet times, it may also result from the fracture dislocation and compression in the spinal if it is congenially narrow. This type of syndrome can also be caused as a result of hematomas and blood build-up.(2)
How to diagnose central cord syndrome?
The doctor performs complete comprehensive neurological examination after taking the patient’s complete medical history. This neurologic exam taking the images of the spinal cord may involve Magnetic resonance imaging(MRI) scan, Computed tomography(CT) scan and X-ray.
MRI scan can explicitly confirm impingement of bone, disc, or hematoma mediated spinal cord. Using strong magnets and computer systems three dimensional pictures can be taken. It demonstrates direct evidence of spinal cord impingement. Findings depend upon the severity of the trauma. Features like cord compression, cord oedema and cord haematoma associated with poor prognosis can be seen.
CT scan of cervical spine shows a narrow spinal canal. It allows the direct approximate degree of spinal cord impingement. A diagnostic image from X-rays of the spine can be produced by a computer in this process. This reveals the size, shape and contents of the spinal canal as well as the surrounding structures.
X-rays produce an image or a film of the spinal region. It shows the vertebral structure and joint borders. The extent of spondylitic change and any dislocations or fractures in the spine can be visualized. The flexion and extension view of X-rays helps to assess the stability of the spinal ligaments.
If vertebral fracture is seen with the central cord syndrome, then neurologic recovery can be different. With vertebral fracture, neurologic deficits are generally more severe, but more early recovery can be seen.(3)
To support the diagnosis of central cord syndrome no specific laboratory blood tests are required.
Treatment
Treatment for central cord syndrome is usually supportive and includes medical and surgical treatment as well as physical therapy. There is no cure for central cord syndrome. Surgical treatment is individualised and indications for it are rare. Through physical therapy the range of motion can be preserved.
Treatment options include:
Non surgical methods
- Occupational and physical therapy
- Neck movement restrictions
- Giving steroids
Neurological symptoms with central cord syndrome can be decreased with conservative therapy
Inpatient treatment
Initial trauma, i.e. first stage of central cord syndrome involves a period of intensive care. Neck collar is used to immobilize the cervical spine and thus prevents further damage to the spine. It continues over 6 weeks until the decrease in the pain and improvement in neurological symptoms. This type of rehabilitation starts usually in the inpatient hospital setting.
Outpatient treatment
After completion of inpatient treatment the patient is discharged and often under goes both occupational and physical therapy. It depends on the extent of injury. The objectives of such type of therapies should be measurable, realistic, specific and time and action oriented.
Using repetitive specific sensory input, movement in patients can be improved. It allows the spinal cord to promote the motor response. The process involves voluntary cycling, strengthening of the muscles, functional electrical stimulation cycling and loco motor training.
Surgical methods
An operation is essential if the patient has greater cervical spine instability. Surgery may be performed for patients with compressed spinal cord fibres. But surgery is needed after a period of recovery. (1) (2)
Prevention
- Always wear a seatbelt whenever you are in vehicle
- Do not drive under the influence of drugs or alcohol
- Use proper equipment and safety measures while playing sports
- Know the depth of the water and dive into it
- Turn in or secure fire arms
- Rearrange objects in house that could cause to trip like wires
Prognosis /Outcomes
- Younger patients of central cord syndrome can expect a good recovery and eventually be able to perform everyday actions
- The prognosis is not so good for elder patients
- If the injury is due to haemorrhage , the prognosis is worse and there are less chances for recovery
- Central cord syndrome resulting from edema leads to paralysis initially which is followed by a quick recovery. This recovery starts from legs and then regain in bladder control and then returns to the function of the arms
- Hand mobility is the final stage of recovery
However, the prognosis mostly depends on the cause of the central cord syndrome. Spontaneous recovery of motor functions is often seen in central cord syndrome patients. (6)
ICD10
The World Health Organization (WHO) published The International Classification of Diseases. Related Health Problems and The International Statistical Classification of Diseases (ICD) provide alpha-numeric codes to classify diseases like symptoms and external causes of injury. Up to six characters long nearly every health condition can be assigned to a unique category and given a code. They usually include a set of similar diseases.
ICD-10-CM S14.126A is grouped within Diagnostic Related Group(s) (MS-DRG v34.0):
- 052 Spinal disorders and injuries with cc/mcc
- 053 Spinal disorders and injuries without cc/mcc
- 955 Craniotomy for multiple significant trauma
- 956 Limb reattachment, hip and femur proc for multiple significant trauma
- 957 Other o.r. procedures for multiple significant trauma with mcc
- 958 Other o.r. procedures for multiple significant trauma with cc
- 959 Other o.r. procedures for multiple significant trauma without cc/mcc
- 963 Other multiple significant trauma with mcc
- 964 Other multiple significant trauma with cc
- 965 Other multiple significant trauma without cc/mcc (5)
References:
- Bernard Robinson, MD, FAANS, Traumatic central cord syndrome: results of surgical management, Journal of Neurosurgery: Spine,July 2002 , Vol. 97, No. 1, Pages 25-32.
- Cortez R, Levi AD. Acute spinal cord injury. Curr Treat Options Neurol. 2007;9(2):115-125.
- Dai L. Magnetic resonance imaging of acute central cord syndrome: correlation with prognosis. Chin. Med. Sci. J. 2003;16 (2): 107-10.
- Harrop, James S; Ashwini Sharan; Jonathon Ratliff (2006). “Central cord injury: pathophysiology, management, and outcomes”. The Spine Journal. 6 (6 Suppl. 1): 198S–206S.
- ICD10data.com
- Office of Communications and Public Liaison,National Institute of Neurological Disorders and Stroke,National Institutes of Health,Bethesda, MD 20892, March 23, 2016.
- Ostrander L. “The Spinal Cord Injured Patient Comprehensive Management, Second Edition”. Demos Medical. (2002) ISBN:188879951X
- Schneider RC, Cherry G, Pantek H (1954). “The syndrome of acute central cervical spinal cord injury; with special reference to the mechanisms involved in hyperextension injuries of cervical spine”. J. Neurosurg. 11 (6): 546–77.
