Trichomoniasis in Men
What is Trichomoniasis in Men
Trichomoniasis is one of the most common sexually transmitted infections (STI) as it affects 3.7 million Americans at any given time. Many of the individuals who have this STI is not aware that they afflicted and transmit it to their partners [1, 2].
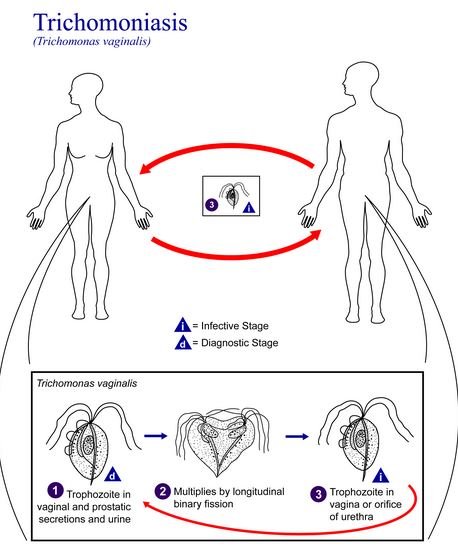
Trichomoniasis is the STI that is caused by the protozoan Trichomonas vaginalis. Humans are the known host of this protozoan and the high prevalence has becoming a public health concern. The transmission of this pathogen is through sexual contact and it is commonly isolated from urethral secretions in male. It has not been obtained from oral sites and the rectal prevalence is found to be low.
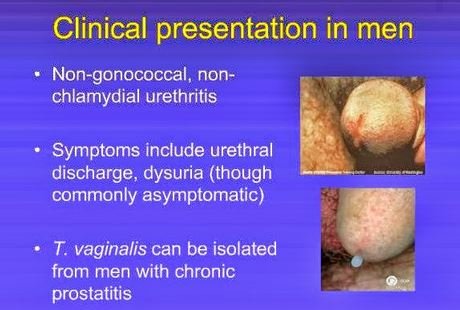
Figure 1 shows the Trichomonas vaginalis protozoan [1, 2, 3, 4].
The protozoan is about the size of a white blood cell though their size may vary with different physical conditions. Once a male is infected, it will be in his anterior urethra, prostate, epididymis, external genitalia and the semen. It lives on the mucosal surface and lumen of the urogenital tract. The flagella of the organism allows it to move around the vaginal tissues [3, 4].
ICD10 code
The ICD-10-CM diagnosis code utilized for trichomoniasis infection is A59.9 [5].
Causes
Being a STI, the Trichomonas vaginalis protozoan is transmitted through sexual contact. As an individual engages in high risk sexual activities, the risk of getting this infection increases [3].
Examples of these activities include:
- Previous STI
- Multiple sexual partners
- Contact with an infected partner
- Use of injection drugs
- Failure to use a barrier contraception such as a condom
Signs & Symptoms of Trichomoniasis in Men
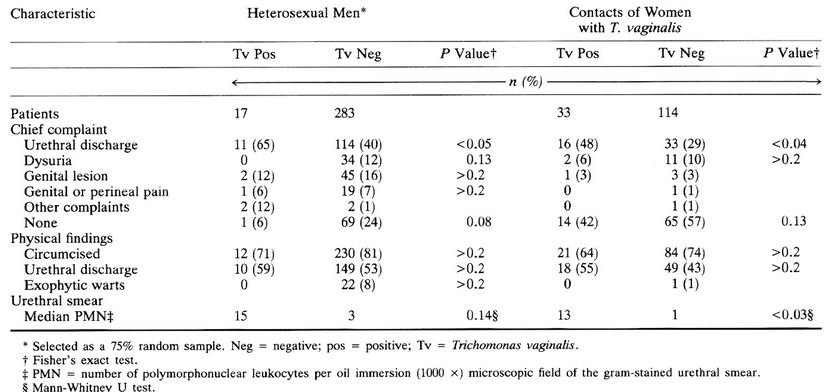
Men who have acquired a trichomonas infection may be categorized into 3 groups [3, 4, 6].
Asymptomatic carrier
Most males do not experience any symptoms, although the pathogen multiplies in their system. They are not aware that T vaginalis is in their system and they unknowingly pass it on to their sexual partners [3, 4].
Mild symptoms
Some of the men may experience mild symptoms such as irritation inside the penis which causes a slight burning feeling during urination or ejaculation. There may also be a mild discharge that comes out of the penis [1, 3, 4].
Acute Trichomoniasis
Those who are in this group report of urethritis which includes dysuria, purulent or mucoid discharge, and urethral pruritus. Pain in the testicles or lower abdomen may be experienced as well. If left unmanaged, this condition may be lead to prostatitis [3, 4].
Diagnosis of Trichomoniasis in Men
Health History and Physical Examination
The patient will seek consultation due to the symptoms that he experienced. The medical history will include the sexual history and engagement in high risk sexual behaviors. Physical examination will start with a visual inspection of the genital area. Epididymitis and prostatitis may occur to these patients. Any penile discharge will be noted by the physician [1, 3, 4].
Culture Test
A culture test is currently the recommended diagnostic test to establish the diagnosis of trichomoniasis. The symptoms of this STI is very similar to others and this test will identify the pathogen to be treated. Urethral swab, semen and urine will be placed in a broth and anaerobically incubated. Growth may be noticed within 48 hours while those without growth after 7 days are considered to be negative for T vaginalis [3, 4].
Treatment of Trichomoniasis
The treatment should be initiated immediately to avoid any complications. If left untreated, the infection may last for months or even years. The oral antibiotic metronidazole is prescribed and must be completed by the individual. It is advisable for both partners to undergo the treatment even if there is no presenting symptoms. They are advised to avoid engaging in sexual activities until the treatment is done.
Those taking metronidazole must be informed to avoid consuming alcohol during the treatment and a few weeks after the treatment. If the individual has complied with the treatment, it would take around 7 days for the infection to be treated. Symptoms which do not improve despite completing the drug treatment should be followed up. Treatment failures may require a susceptibility test from the CDC [1, 3, 4].
Prevention of Trichomoniasis
Even after completing the treatment, it is still possible to contract Trichomoniasis again. Based on statistics, around 20% of those who have received treatment were re-infected within 3 months. Abstaining from any sexual intercourse is the best way to prevent contracting the infection again. If this can’t be done, the use of barrier protection such as condoms to reduce the risk for infection [1, 3].
It is also advisable to limit the number of sexual partners and avoid multiple partners at the same time. The use of spermicides are not recommended for prevention of STIs and the frequent use of these may damage the epithelium of the genitals and increased the risk for getting HIVs or other STIs. Any suspected symptoms should be referred to the physicians to prevent the spread of infection to others [1, 3, 4].
References
- Centers for Disease Control and Prevention. (2015, November 17). Trichomoniasis- CDC Fact Sheet. Retrieved from Centers for Disease Control and Prevention: http://www.cdc.gov/std/trichomonas/stdfact-trichomoniasis.htm
- Reed-Guy, L. (2016, January 29). Trichomoniasis. Retrieved from Healthline: http://www.healthline.com/health/trichomonas-infection
- Smith, D. S. (2015, October 21). Trichomoniasis. Retrieved from eMedicine: http://emedicine.medscape.com/article/230617-overview
- Johnson, T. (2015, November 19). Trichomoniasis. Retrieved from WebMD: http://www.webmd.com/sexual-conditions/guide/trichomoniasis?page=2
- (2015). Trichomoniasis, unspecified. Retrieved from ICD10Data: http://www.icd10data.com/ICD10CM/Codes/A00-B99/A50-A64/A59-/A59.9
- I Wanna Know. (2015). Trichomoniasis. Retrieved from I Wanna Know: http://www.iwannaknow.org/teens/sti/trichomoniasis.html
