Trichomonas Vaginalis
What is Trichomonas Vaginalis?
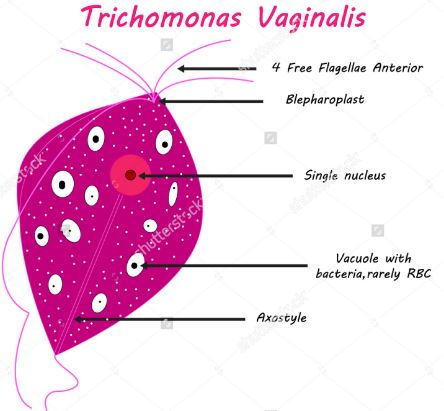
Trichomonas vaginalis or TV is an infective agent and characteristically classified under parasitic protozoan (plural – protozoa). TV causes sexually transmitted disease (STD) known as trichomoniasis. TV enters into the genital organ, including the vagina, urethra or underneath the foreskin and infection develops.
Early intervention can cure the infection completely, but the untreated condition has many perinatal complications. Both male and female can affected with this infection and develops genitourinary tract infections, and most common risk is HIV transmission, though trichomoniasis is a non-viral infection. (1,3)
Symptoms
Some Trichomonas vaginalis infection does not provide any symptoms and affected persons (male or female) can pass on the infection to their sexual partner. Yet now the proper cause of the difference of asymptomatic and symptomatic cases is unclear, but it may vary depending upon the age or other health condition.
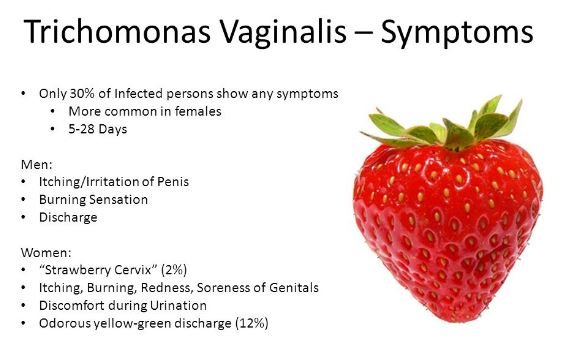
The included symptoms are described below.
In female
- Vaginal discharge become frothy
- Volume of vaginal discharge is increased
- Smelly discharge from vagina
- Burning sensation during urination
- Itching
- Inflammation
- Pain during sexual intercourse
In male
- Penis tip secretes a discharge
- Burning sensation during urination
- The urge of the urination increased
- Foreskin is inflamed and tenderness develops (1,2)
Mode of transmission of Trichomonas vaginalis
The transmission of TV occurs during sexual intercourse, The infection causing protozoan is usually transmitted from a vagina to penis, or from a penis to a vagina. But lesbians are equally has the risk of transmission of TV as it can pass from a vagina to another vagina. The certainty is very less that the parasite can infect the mouth, hands, or anus during love making. The following are the modes of transmission, through which TV can enter into genitourinary tract:
- Unsafe love making or sexual intercourse without using condom
- Finger insertion into the vagina
- Multiple user of same sex toys
- TV can transfer to neonates during vaginal childbirth
However, Trichomonas vaginalis cannot transmit from toilet seats or swimming pools sharing cloths and hugging.
Risk factors of trichomoniasis
Female are more susceptible than male and incidence are more in older aged female than young aged female. The following risk factors are applicable for both male and female:
- Sex workers, who make sexual relation with multiple partners
- Vulnerable subject who frequently affected with other sexually transmitted infections
- A previous medical history of trichomoniasis
- Unprotected sex or sexual intercourse without a condom
T. vaginalis can make complicated Pregnancy
If pregnant women get infected with TV, then common associated incidences include
- Placental membranes become prematurely ruptured
- Premature delivery, and
- Neonates have low-birth-weight, usually less than 5.5 pounds. (1,3)
Complications associated with trichomoniasis
The infected person with a T. vaginalis infection has an enhanced propensity towards HIV (human immunodeficiency virus) infection. This conclusive statement is developed due to researchers found that the female prostitutes who has HIV seroconversion, they are significantly associated with the trichomoniasis or other STDs. It is assumed that trichomoniasis may cause confined growth of HIV- contaminated or HIV- liable cells, such as lymphocytes and macrophages, which augment the transmission of HIV.
Trichomoniasis is also has association with cervical cancer, atypical pelvic inflammatory disease, and infertility. (1, 3, 4)
Diagnosis
The accurate diagnosis is very important as TV is associated with asymptomatic manifestation. Inaccurate diagnosis is also increased the scope of other mentioned complications. Proper diagnosis can control the spreading of infection and reduce the scope of complications. The following diagnostic tests help to identify the T. vaginalis.
- Culture media and Microscopic examination of urine or vaginal swab is a cost effective method to diagnose the TV. This test has some limitations like does not provide quick result, etiologic detection of TV is difficult.

- Antibody based technique is considered as an advance method of detecting vaginalis. To conduct this test, blood sample is collected from the infected person. But it also has some limitation, as trichomonal antibodies may persevere for a prolonged time after treatment. Therefore, existing and earlier period infections cannot be evaluated properly.
- DNA techniquesis a superior version of diagnosis of vaginalis, as it helps to encounter the false or negative results. This can able to identify the asymptomatic cases. (2)
Treatment
Early and accurate detection has provided complete cure from T. vaginalis infection. The prescription of treatment usually contains antibiotic therapy.
The drug of choice to treat T. vaginalis infection is metronidazole or tinidazole. Doctor prescribed to take the antibiotic therapy for both the partners.
The usual therapy is continued for 7 days. If symptoms do not disappear, then a second course of antibiotic need to complete eradication of infection.
Both the antibiotic do not interfere with contraceptive pills or pregnancy. Doctors usually suggest to avoid alcohol consumption at least 48 hours after the completion of the whole course of the treatment, as it will create nausea and vomiting. (1,3)
References
- BASHH (2014); Trichomonas Vaginalis; Retrieve from: http://www.bashh.org/documents/TV%20PIL%20Screen%20-%20Edit.pdf
- Dino Petrin, Kiera Delgaty, Renuka Bhatt, and Gary Garber (1998); Clinical and Microbiological Aspects of Trichomonas vaginalis; Retrieve from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC106834/
- Centers for Disease Control and Prevention (2015); Trichomoniasis – CDC Fact Sheet; Retrieve from: http://www.cdc.gov/std/trichomonas/stdfact-trichomoniasis.htm
- Lauren Reed-Guy; Trichomoniasis; Retrieve from: http://www.healthline.com/health/trichomonas-infection
