Heliotrope Rash
What is heliotrope rash?
Heliotrope rash is a characteristic symptom of Dermatomyositis. Dermatomyositis is idiopathic inflammatory myositis which causes persistent inflammation on the muscle and skin. The heliotrope rash is developed on the upper eyelids and become inflamed. Usually the condition is associated with violaceous erythema of the upper eyelids, in addition edema and telangiectasia also progress in the heliotrope rash.
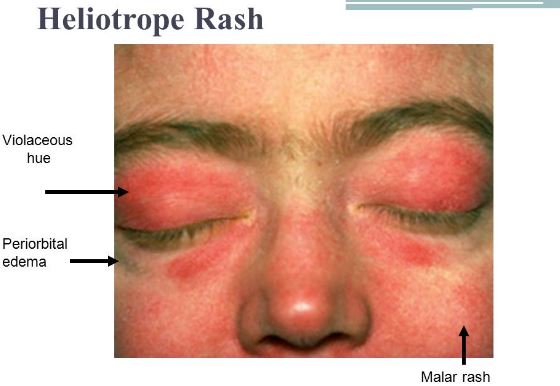
The term ‘ heliotrope’ is derived from the heliotrope flower, as in this rash skin coloration is changed to violet color. (1,2)
Associated symptoms of heliotrope rash
Heliotrope rash is developed due to the onset of idiopathic inflammatory myositis, specifically in dermatomyositis. The characteristic feature of Heliotrope rash is violaceous discoloration and periorbital edema. Skin becomes itchy with ragged cuticles. Fatigue muscle is also developing with Heliotrope rash. Other than this the associated symptoms are:
Gottron’s sign
Gottron’s sign is developed in the knees, elbow and fingers. The included characteristics of this symptom are red, flat rash occurs on the backside of the knees, elbow and fingers.
Gottron’s papules
This is similar as Gottron’s sign, but instead of flat, this produces scaly bumps develops on the finger’s joints.
Shawl sign
The characteristic feature of shawl sign reddish purple flat discoloration spread over wide part of the skin including neck, shoulders, arm etc. Sun exposure can worse the condition due to ultraviolet rays.
V-sign
This is similar as shawl sign, but it develops at the chest and the shape of the rash looks like a v-necked shaped sweater.
Reddish nail bed
The finger nail bed become reddish due to inflammation of the surrounding blood vessels.
Mechanic’s hands
The appearance of the hands becomes dirty, as the skin of the hand has cracked, roughed, brittle nails with irregular tips and side of the nails. The hands appear as manual mechanics. (1,2)
Causes
The following are the causes of development of the Heliotrope rash:
Dermatomyositis (DM)
This is the clinical condition in which skin rash along with skeletal muscle become inflamed.
Juvenile dermatomyositis (JDM)
This condition is similar as dermatomyositis, but affects in children.
Amyopathic dermatomyositis (ADM)
In this condition, only cutaneous tissues are involved without affects the muscles and different types of rashes are common symptoms.
The possible causes of development of the above mentions clinical conditions are:
- Genetic abnormality
- Skin malignancy
- Exposure of toxic chemicals or natural infectious agent
- Side effect of certain drugs including penicillamine, quinidine, phenylbutazone, hydroxyurea and statin. (3,4)
Diagnosis
The following tests are conducted for determining the underlying disease condition:
- Skin biopsy
- Enzymatic testing includes estimation of creatine kinase, lactic dehydrogenase, alanine aminotransferase or aldolase. The elevated level of creatine kinase and lactic dehydrogenase help to detect the condition.
- Serologic tests such as positive finding of antinuclear antibody testing helps to detecting The biomarker of ADM is 155-kd antigen or Se antigen (90-95 kd), and detecting of this also helps to identify the cause. For benefit of clinical prospect, serologic testing for myositis-specific antibodies is beneficial.
- Von Willebrand factor detection for diagnosing the JDM.
The above mention tests are conducted for confirming the underlying cause and the bellow mentioned tests are conducted for analysis the severity of the condition:
- Esophageal motility studies and/or swallowing evaluation for assessing the involvement of the esophagus.
- Chest X-ray and pulmonary function test is conducted for evaluation of lung involvement.
- Electrocardiogram is also performed to analysis the cardiac functionality. (3,4,5)
Treatment
The treatment depends upon the diagnostic test result. The following treatment options are available:
- Complete rest with adequate stretching and splinting physical manipulation helps to manage the muscle weakness.
- Avoidance of direct sunlight is highly recommended.
- High SPF and ultraviolet ray protecting sun- screen and protective accessories and clothing are recommended during exposure to sunlight.
- For reduction of skin inflammation and itching, anti-histaminic ointment can provide beneficial effects.
- Steroidal drugs including corticosteroids, prednisone are prescribed. The dose is dependent on body weight. Usually steroidal therapy helps to provide complete remission. If the condition is recurred, then restart the steroidal therapy.
- Immunosuppressive agents including methotrexate, cyclophosphamide, azathioprine, cyclosporinare chlorambucil or mycophenolate mofetil prescribed as maintenance therapy or preventing the recurrence.
- Pimecrolimus cream (1%) or tacrolimus ointment (0.1%) are acts as immunomodulator and helpful to treat symptoms associated with cutaneous tissue.
- Antihypertensive drugs are prescribed, if cardiac association is prominent. (4, 5)
Pictures



References
- Marc L Miller (2015), Patient information: Polymyositis, dermatomyositis, and other forms of idiopathic inflammatory myopathy (Beyond the Basics); Retrieve from: http://www.uptodate.com/contents/polymyositis-dermatomyositis-and-other-forms-of-idiopathic-inflammatory-myopathy-beyond-the-basics
- Prashanth Sunkureddi (et al) (2005); Signs of Dermatomyositis; Retrieve from: http://www.turner-white.com/memberfile.php?PubCode=hp_apr05_signs.pdf
- RIC ANTHONY KOLER, ANDREW MONTEMARANO (2001); Dermatomyositis; Retrieve from: http://www.aafp.org/afp/2001/1101/p1565.html
- DermNet NZ (2015); Dermatomyositis; Retrieve from: http://www.dermnetnz.org/immune/dermatomyositis.html
- Jeffrey P. Callen, Robert L. Wortmann, (2006);Dermatomyositis; Retrieve from: http://www.myositis.org/storage/documents/DM_Published_Research/Dermatomyositis_by_Callen_and_Wortmann.pdf
