Placenta Percreta
Placenta percreta is a type of medical condition wherein the placenta implants itself too deep into the uterus. This situation is life-threatening to both the mother and the fetus and it usually requires a multi-disciplinary treatment [1, 2].
What is Placenta Percreta?
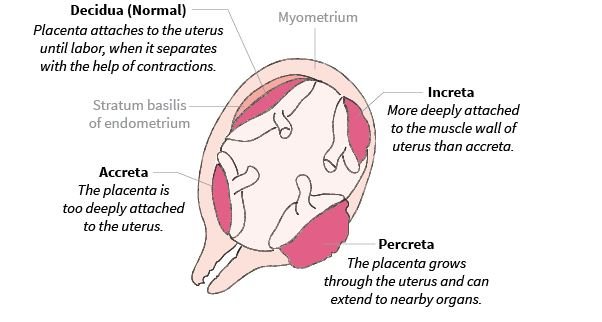
The term placenta accreta is used to describe the event wherein the placenta, or a part of it, attaches too deeply into the uterus and becomes inseparable from the uterine wall. There are several types of this condition depending on the degree of attachment of the placenta.
When the placenta invades the myometrium only, the term placenta increta is used. But if the attachment goes deeper than the myometrium and involves adjacent organs such as the bladder, the condition is called placenta percreta.[1, 2, 3].
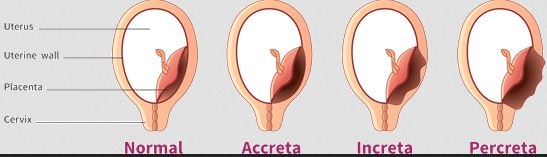
Figure 2 shows the normal attachment of the uterus and what occurs in different types of placenta accreta
Placenta percreta is considered to be the least common and the most severe type of placenta accreta. In this condition, the vascular processes of the placenta, called chorionic villi, invades not only the full thickness of the myometrium but also the outermost covering of the uterus called serosa. There are times that the placenta attaches itself to other organs. Some of the organs that are usually affected are the rectum and the bladder [4, 5].
ICD-10 code for Placenta percreta
The 2016 ICD-10-CM diagnosis code utilized for placenta percreta is O43.23. The number 1, 2 or 3 is added at the end of the end to specify if the patient is in in the first, second or third trimester respectively. The number 9 is added if the trimester the patient in is unknown [6].
Risk Factors
The exact cause of placenta percreta is unknown but there are several factors that increases the risk of an invasive placenta.
Previous Cesarean Delivery
A history of a previous delivery through a cesarean section is considered to be the greatest risk factor and this risk further increases with the number of cesarean deliveries the patient had undergone. The risk is related to the scar that is left on the internal uterine surface after the c-section. The endometrium over this scar is thinner and this may become the site of the invasive placental implantation [1, 7].
Previous Uterine Surgeries
Any uterine surgeries in the past puts the female at risk due to the scarring that it causes on the surface of the uterus. Examples of these surgical procedures are dilatation and curettage and hysteroscopy myomectomy [7].
Placenta Previa
Placenta previa is the condition where the placenta blocks the neck of the uterus and this had interfered the supposedly normal delivery of the baby. This sometimes result to scarring in the uterus and may increase the possibility of placenta percreta [1].
Signs
Usually, there are no signs or symptoms that are associated with this condition while a woman is going through the pregnancy. The diagnosis is only made when the placenta is attempted to be removed after the delivery [7].
Diagnosis
Any attempt to remove the placenta may cause any bleeding, so it will be ideal to make the diagnosis antenatally in order to make the necessary preparations. A woman who is at risk for having an invasive placenta may be requested to undergo imaging tests to assist in making the diagnosis [1, 2, 7].
Imaging Tests
Ultrasounds are perform first to analyze the texture of the placenta and its border with the uterine muscle. If an abnormality is suspected, a Magnetic Resonance Imaging scan (MRI scan) will be able to provide a visualization of the placenta to establish the diagnosis of an invasive placenta [1, 7].
Treatment
Once the suspicions of a placenta percreta is confirmed, a multi-disciplinary team will be formed as preparation for the delivery. Women may be referred to a specialized tertiary center for the actual delivery. The team may be composed of an anesthesiologist, obstetrician, neonatologist and hematologist.
There is a risk of a massive hemorrhage and this will be prepared as well. Depending on the nature of the damage to the uterus, there may be a need to perform a hysterectomy after the delivery. Surgical options should be discussed with the obstetrician especially if there are plans to have more children in the future [1, 2, 7].
References
- American Pregnancy Association. (2015, August). Placenta Accreta. Retrieved from American Pregnancy Association: http://americanpregnancy.org/pregnancy-complications/placenta-accreta/
- American College of Obstetricians and Gynecologists. (2012). Placenta Accreta. Retrieved from American College of Obstetricians and Gynecologists: http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Placenta-Accreta
- Focus Information Technology. (2014). Placenta Accreta. Retrieved from Perinatology.com: http://perinatology.com/wordpress/?p=109
- (2012, March 19). Definition of Placenta percreta. Retrieved from MedicineNet: http://www.medicinenet.com/script/main/art.asp?articlekey=4921
- Konijeti, R., Rajfer, J., & Askari, A. (2009). Placenta Percreta and the Urologist. Reviews in Urology, 173-176.
- (2015). Placental Disorders. Retrieved from ICD10Data: http://www.icd10data.com/ICD10CM/Codes/O00-O9A/O30-O48/O43-
- Windrim, R. (2015). Invasive Placenta. Retrieved from Mount SInai Hospital: http://www.mountsinai.on.ca/care/placenta-clinic/complications/invasiveplacenta
