Mixed Connective Tissue Disease
What is mixed connective tissue disease?
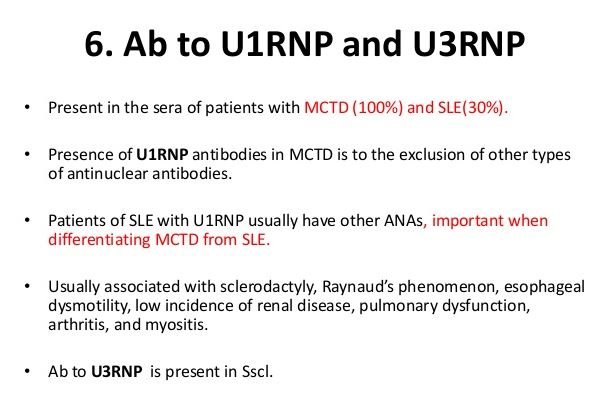
Mixed connective tissue disease (MCTD) is a combination of characteristics, which are symptomatic features of primarily lupus, scleroderma and polymyositis. It is one type of rheumatic disease where all the symptoms are overlapping and terms as overlap disorder. This disease affects the fundamental cells of the body. U1-ribonucleoprotein (RNP) and antinuclear antibodies is developed in the blood which acts against antibody. All the symptoms are not arises at a time and in due course of time they progress and dominated with other symptoms. (1,2)
Symptoms of MCTD
The symptoms are not same for every affected individual, it differs depending upon the dominating features of the affected disease. However, individual suffers from MCTD does not have severe symptoms in comparison with a person affected with any selected single disease.
- Muscle weakness is prominent for dominant feature of polymyositis.
- Chest pain along with breathing problem kidney problem and/ or arthritis are the common symptoms of primarily lupus.
- Bulge and keratogenic effects are prominent in the fingers and sole of the feet. During cold exposure, bluish discoloration of the fingers are also common.
Other than these some specific features are common in MCTD:
Raynaud’s phenomenon
In cold exposure, the blood vessels of hands and feet become constricted or dilated, which can be characterized by painful, bulging fingers and toes with lower temperature in hand and feet.
Polyarthralgia with inflammation
The symptoms of polyarthralgia is characterized by multiple joint pain and inflammation. The symptoms are quite similar with rheumatoid arthritis. Muscle weakness is also common, as myopathy (swelling of the muscle fibers) is developed and may associated with tenderness. Fever and fatigue can also present.
Edema
Accumulation of the fluid in the finger joints is common and cause bulging of the fingers.
Symptoms developed in the skin
Reddish or reddish brown patches, violet discoloration of the eyelids, alopecia (hair loss) and periungual telangiectasia (the blood vessels present around the fingernails become dilated).
Internal organ dysfunctionality
- Hypomotility means esophageal dysfunction is a common symptom in MCTD. Respiratory dysfunction and pulmonary hypertension are associated problems due to lung function disorder.
- Onset of MCTD in childhood can cause aortic insufficiency, myocarditis and pericarditis, whereas cardiac disorder is less common in adult.
- Mild kidney related dysfunctions are associated, but in rare cases the major renal problem may occur.
- Neurological disease, including cognitive dysfunction, meningitis, trigeminal sensory neuropathy, headache and cerebral thrombosis can also associate with MCTD.
- The low level of the total blood count (TLC) indicates anemia (insufficient RBCs), leukopenia (insufficient WBCs) are also associated with MCTD. Splenomegaly (enlargement of the spleen), hepatomegaly (enlargement of the liver) and intestinal disorders are also associated with MCTD. (3,4)
Causes & Pathology
The precise cause of MCTD is yet not understood fully, but it assumed that abnormality in the immune system or genetic disorder may involve in the development of MCTD.
The evidence supports that higher level of antinuclear antibodies (ANAs) is a common finding of MCTD, which affect ribonucleoprotein (anti-RNP).
Abnormal pathophysiological changes find in MCTD are, as follows:
- Anti–U1-70 kd and anti–U1-RNP autoantibodies are in high level due to hyperactivity of the B-lymphocyte.
- In the peripheral blood, circulating anti–U1-70 kd–reactive T lymphocytes are present due to T-lymphocyte activation.
- Apoptotic alteration occurs in U1-70 kd antigen
- Apoptotically alteration in self-antigens develop due to immune response.
- Genetic involvement occur with chief histocompatibility genes i.e. human leukocyte antigen
- Proliferation with vascular endothelial tissue develops along with extensive lymphocytic and plasmacytic infiltration of tissues. (2, 4)
Diagnosis
The symptomatic analysis is very important to diagnose the MCTD and if doctor suspects the MCTD, then following tests may need to conduct
- Blood test is conducted for estimation of involved antibodies and rheumatoid factors is needed for
- For evaluation of electric impulse activity in the muscle fibers. This test helps to identify the communication between neuron and muscles.
- Biopsy of the muscular tissue. This test is conducted by taking the sample of muscular tissue and examine under microscope. Presence of muscle damage indicates the presence of MCTD. (5)
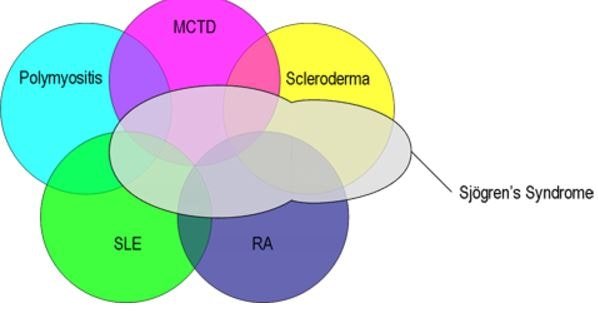
Differential diagnosis of mixed connective tissue disease
Treatment
- For treating the lupus symptoms early incorporation of corticosteroids are helpful.
- Non-steroidal- anti-inflammatory drugs are prescribed for treating mild inflammation and joint pain
- Severe inflammatory condition can be treated with prednisone or other steroidal drugs.
- TNF blockers are prescribed for the management of the arthritis.
- Immunosuppressive drugs are used to control the disease.
- For treatment of Raynaud’s phenomenon, calcium channel blockers are widely used.
- Captopril, enalpril are prescribed for cardiac disorder, especially for the management of hypertension.
- Antimalarial drugs are prescribed for treating the fever.
- Proton pump inhibitor (Omeprazole) or antacids are recommended for frequent heartburn. (1,3,4)
Prognosis
The severity of the MCTD depends upon which organs involved. Early diagnosis and treatment can provide better prognosis (3).
Life expectancy
Depending upon the organs affected with MCTD or delaying of the initiation of treatment are the two major factors for determining the life expectancy. Mild cases with early diagnosis and treatment provides better outcome and life expectancy (3).
References
- Mayo Clinic Staff (2015); Mixed connective tissue disease; Retrieve from: http://www.mayoclinic.org/diseases-conditions/mixed-connective-tissue-disease/basics/definition/con-20026515
- Eric L Greidinger (2015); Mixed Connective-Tissue Disease; Retrieve from: http://emedicine.medscape.com/article/335815-overview
- William C. Shiel Jr. (2015); Mixed Connective Tissue Disease; Retrieve from: http://www.medicinenet.com/mixed_connective_tissue_disease/page2.htm
- National Organization for Rare Disorders (2007), Mixed Connective Tissue Disease (MCTD); Retrieve from: http://rarediseases.org/rare-diseases/mixed-connective-tissue-disease-mctd/
- Rula A. Hajj-ali (2015), Mixed Connective Tissue Disease (MCTD); Retrieve from: http://www.merckmanuals.com/home/bone,-joint,-and-muscle-disorders/autoimmune-disorders-of-connective-tissue/mixed-connective-tissue-disease-(mctd)
