Dyslipidemia
What is Dyslipidemia?
Dyslipidemia is a condition where there is an abnormal amount of lipids found in blood, either cholesterol or fat. Cholesterol is an important fatty substance utilized by the body to produce some hormones and metabolize food.
The very common type is hyperlipidemia which refers to the elevation of lipid levels in the blood stream, usually due to diet and lifestyle. Prolonged elevation of insulin levels especially among diabetic patients can also lead to this condition. The increased levels of O-GIcNAC transferase (OGT) may also lead to dyslipidemia. OGT is a gene responsible for the resistance of insulin in muscle cells.
Dyslipidemia can be classified according to phenotype or in its etiology. Phenotype is its presentation in the body; especially the specific type is not within the normal level. Etiology is the main reason why the condition occurs, whether it is genetic in nature or it’s secondary to another health problem.
Clinical Signs and Symptoms of Dyslipidemia
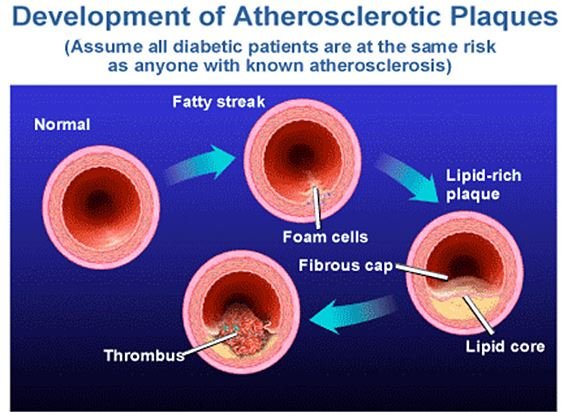
Dyslipidemia has no specific clinical symptoms, but it has the tendency to cause vascular disease, such as coronary artery disease (CAD), stroke and peripheral arterial disease. Increased levels of triglycerides (TGs) can result to acute pancreatitis.
Increased levels of low-density lipoprotein (LDL) can result to arcus corneae and tendinous xanthomas at the arc of Achilles, elbow, knee tendons and at the metacarpophalangeal joints. This can be seen among patients who develop familial hypercholesterolemia, associated with the rising of planar or tuberous xanthomas.
Planar xanthomas appears flattened while some are lightly raised yellowish patches of the patient’s skin; whereas tuberous xanthomas are painless, firm nodules found over the extensor surfaces of joints. Patients with increased levels of TGs can have the eruptive type of xanthomas on their trunk, back, elbows, buttocks region, knees, and in the upper and lower extremities.
Patients with the rare type of dysbetalipoproteinemia can present signs of palmar and tuberous xanthomas. Severe hypertriglyceridemia can lead to a creamy white appearance of the retinal arteries and veins. A very high level state of lipid levels can give the blood plasma its lactescent appearance. Individuals with these can have paresthesias, dyspnea and confusion.
Primary and Secondary Causes of Dyslipidemia
The etiology of dyslipidemia can be due to primary causes or secondary causes. Primary causes are those which are basically genetic in nature; secondary causes are those related with a person’s lifestyle habits, as well as other possible reasons, like existence of other health conditions. All of these can result to the development of dyslipidemia in varying degrees.
Primary Causes
These are the single or multiple mutations among genes which lead to either of the following; overproduction or defective clearance of TG and LDL cholesterol, or the much decreased production or excessive clearance of high-density lipoprotein (HDL). An example of this is the familial hypercholesterolemia.
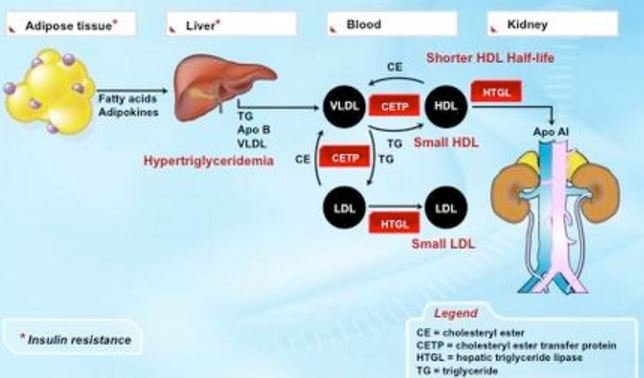
Image 2 – Normal Lipids or fat metabolism
Secondary Causes
These are known to be the most contributory factor with several cases of dyslipidemia among adult individuals. It is accounted to a sedentary lifestyle with an excessive dietary intake of saturated form of fats, cholesterol and trans fats. Other secondary causes include the following health conditions:
- Diabetes mellitus
- Hypothyroidism
- Nephrotic syndrome
- Primary biliary cirrhosis
- HIV infection
- Obesity
- Chronic kidney disease
- Cigarette smoking
- Alcohol overuse
- Cholestatic liver diseases
- Drugs such as estrogen and progestins, thiazides, retinoids, cyclosporine, highly active antiretroviral agents, β-blockers, tacrolimus, anabolic steroids and glucocorticoids
Diagnostic Examinations and Procedures
Serum lipid profile is evaluated by measuring the total cholesterol, TG, and HDL cholesterol and calculated LDL cholesterol and VLDL in blood.
There are three measurements used to assess the overall lipid profile status in a person’s body:
- Low-density lipoprotein (LDL) or the bad cholesterol. An elevated LDL can place someone at risk to develop a cardiovascular disease. The higher is the level of the LDL, the greater is the chance that the patient is at risk to have a heart problem.
- High-density lipoprotein (HDL) or the good cholesterol. This type removes the bad cholesterol from one’s body by bringing it back to the liver. An increased level of HDL protects a patient against the formation of any heart disease.
- Triglycerides are the fat deposits which are found in blood. Patients got these from the fat of the food they eat, such as from vegetable oil and animal fats. The higher is its level in blood, the more that a person is having the chance to have a cardiovascular disease.
Screening tests are done to all individuals who are at risk to develop the problem and to those with other causes of the disease.
Medical Treatment and Management
Treatment is necessary for all patients who have cardiovascular disorders, either for primary or secondary preventive measures. The general management is based on these options:
- Risk assessment for children and adult patients has to be discussed with them
- Significant lifestyle changes have to be emphasized, like regular exercise regimen and some dietary modification schedule
- Patients with high LDL cholesterol are given with statins, bile acid sequestrants, niacin, ezetimibe, and other measures
- Patients with high TG are given with niacin, omega-3 fatty acids, fibrates, and other measures
ICD9 Code for Dyslipidemia
The ICD9 Code for disorders of lipid metabolism is 272 and specified as follows:
- 272.0 Pure hypercholesterolemia
- 272.1 Pure hyperglyceridemia
- 272.2 Mixed hyperlipidemia
- 272.3 Hyperchylomicronemia
- 272.4 Other and unspecified hyperlipidemia
- 272.5 Lipoprotein deficiencies
- 272.6 Lipodystrophy
- 272.7 Lipidoses
- 272.8 Other disorders of lipoid metabolism
- 272.9 Unspecified disorder of lipoid metabolism
References
- http://www.msdmanuals.com/professional/endocrine-and-metabolic-disorders/lipid-disorders/dyslipidemia
- http://www.hopkinsmedicine.org/digestive_weight_loss_center/conditions/high_cholesterol.html
- http://www.uptodate.com/contents/secondary-causes-of-dyslipidemia#H1
- Vodnala D, Rubenfire M, Brook RD (2012). Secondary causes of dyslipidemia. Am J Cardiol; 110:823.
- Garvey WT, Kwon S, Zheng D, et al (2003). Effects of insulin resistance and type 2 diabetes on lipoprotein subclass particle size and concentration determined by nuclear magnetic resonance. Diabetes. 52:453.
- Park H, Kim K (2012). Association of alcohol consumption with lipid profile in hypertensive men. Alcohol. 47:282.
